Gynecomastia
Gynecomastia, also known as gyno is a condition often shrouded in misconception and embarrassment, affects males of all ages and backgrounds. While it might be considered a minor or cosmetic concern, gynecomastia can have profound physical and psychological effects on those who experience it. In this comprehensive article, we delve into the intricacies of gynecomastia, exploring its causes, symptoms, potential health implications, and available treatments
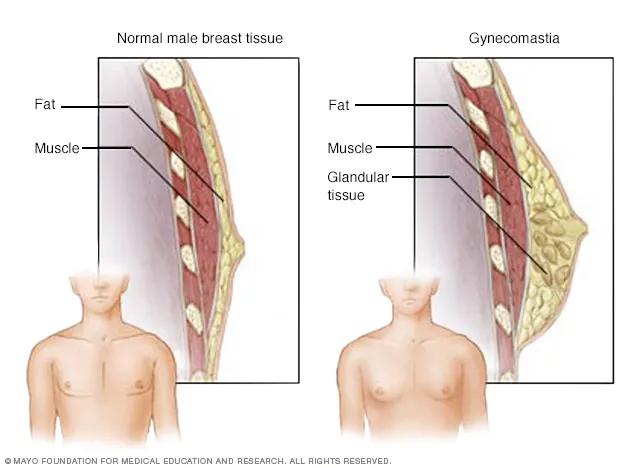
What is Gynecomastia?
Gynecomastia is a medical condition characterized by the enlargement of breast tissue in males. It can result in the appearance of breasts that are larger or more prominent than what is typical for males. Gynecomastia can affect one or both breasts and can occur at any age, from infancy to adulthood. It is important to note that gynecomastia is different from the temporary breast enlargement that can occur during puberty in some boys, which typically resolves on its own.
What causes gyno?
Gyno can be caused by various factors that disrupt the hormonal balance between estrogen and testosterone, leading to the growth of breast tissue. Here are some of the primary causes of gynecomastia:
Hormonal Changes During Puberty: Hormonal fluctuations during puberty can lead to temporary gynecomastia. As the body undergoes changes, there can be a temporary imbalance between estrogen (female hormone) and testosterone (male hormone), resulting in breast tissue growth. This type of gynecomastia often resolves on its own within a few months to a couple of years.
Hormonal Imbalances: Hormonal imbalances can occur at any age and result from conditions that disrupt the normal production of hormones. Conditions such as hypogonadism (low testosterone), hyperthyroidism (overactive thyroid), and hypothyroidism (underactive thyroid) can contribute to gynecomastia.
Medications: Some medications can cause gynecomastia as a side effect. These include:
- Anti-androgens used in prostate cancer treatment.
- Some anti-anxiety medications.
- Certain antipsychotics.
- Medications used to treat heart conditions, including digoxin and calcium channel blockers.
- Some anti-HIV medications.
- Anabolic steroids and androgenic prohormones.
Illicit Drug Use: Use of certain recreational drugs, such as marijuana, heroin, and methadone, can lead to gynecomastia.
Medical Conditions: Certain medical conditions can contribute to gynecomastia. These include kidney failure, liver disease, and certain tumors that affect hormone production.
Aging: As men age, their testosterone levels may decline while estrogen levels remain relatively stable. This shift in hormonal balance can lead to gynecomastia in older individuals.
Genetic Predisposition: Some individuals may have a genetic predisposition to developing gynecomastia, especially if there’s a family history of the condition.
Lifestyle Factors: Excessive alcohol consumption and the use of anabolic steroids or performance-enhancing substances can increase the risk of gynecomastia.
Weight Gain: In some cases, excess weight and obesity can lead to an increase in estrogen levels, contributing to the development of gynecomastia.
It’s important to note that gynecomastia can have various causes, and sometimes multiple factors may contribute simultaneously. If you suspect you have gynecomastia, it’s recommended to consult a healthcare professional for an accurate diagnosis and appropriate treatment options based on the underlying cause.
Does gyno go away?
In many cases, gynecomastia can go away on its own, especially if it is related to temporary hormonal fluctuations such as those that occur during puberty. However, whether gynecomastia goes away depends on several factors, including the underlying cause, the individual’s age, and the duration of the condition.
It’s important to emphasise that every individual’s experience with gynecomastia is unique. If you suspect you have gynecomastia, it’s recommended to consult a healthcare professional for a proper diagnosis and guidance. They can help determine the underlying cause of the condition and recommend appropriate treatment options based on your individual circumstances and needs.
What are the treatment options for gynecomastia?
Treatment options for gynecomastia vary depending on the underlying cause, the severity of the condition, and the individual’s preferences. Here are some common treatment approaches:
Observation and Lifestyle Changes:
- In cases where gynecomastia is mild and attributed to factors like puberty, weight gain, or certain medications, healthcare professionals may recommend observation and lifestyle changes.
- Losing excess weight through a balanced diet and regular exercise can help reduce the amount of adipose (fat) tissue, potentially improving the appearance of the chest.
Medication:
- Medications may be considered in cases of persistent or more severe gynecomastia. These medications work by altering hormonal balance:
- Selective Estrogen Receptor Modulators (SERMs) like tamoxifen and raloxifene can help block the effects of estrogen on breast tissue.
- Aromatase inhibitors (such as anastrozole) can reduce the production of estrogen.
- Medications may be considered in cases of persistent or more severe gynecomastia. These medications work by altering hormonal balance:
Hormonal Therapy:
- In cases of significant or persistent gynecomastia, hormonal therapy under medical supervision might be considered. This involves using medications to restore hormonal balance by increasing testosterone levels or decreasing estrogen levels.
Surgery:
- Surgical intervention is often considered when gynecomastia does not respond to conservative treatments or causes significant physical or emotional distress.
- Liposuction: In cases where gynecomastia is primarily due to excess fat, liposuction can be used to remove fatty tissue and sculpt the chest.
- Excision: In cases where glandular tissue is the primary cause of gynecomastia, surgical excision of the tissue is performed to achieve a flatter chest contour. This procedure is typically performed under local or general anesthesia.
- Combination Procedures: In some cases, a combination of liposuction and excision may be used to address both fat and glandular tissue.
Psychological Support:
- Gynecomastia can have significant psychological impacts, leading to body image concerns and emotional distress. Psychological support, counseling, and support groups can play an essential role in managing the emotional aspect of gynecomastia.
How to prevent gyno when on cycle
If you are considering anabolic steroid or prohormone cycles that might potentially lead to gynecomastia (gyno), it’s important to take steps to minimise the risk. Gynecomastia is often associated with hormonal imbalances, specifically increased levels of estrogen relative to testosterone. Here are some strategies that individuals may consider to help prevent gynecomastia while on a cycle:
Selective Estrogen Receptor Modulators (SERMs):
- SERMs like tamoxifen and raloxifene can help block the effects of estrogen in breast tissue. They are often used as preventive measures or treatments for gynecomastia during and after a cycle.
- Consult a healthcare professional before using any medications, as they can provide guidance on dosage and duration.
Aromatase Inhibitors (AIs):
- Aromatase inhibitors, such as anastrozole and letrozole, reduce the conversion of testosterone into estrogen. These can help control estrogen levels during a cycle.
- It’s important to use AIs under medical supervision, as excessive suppression of estrogen can have negative effects on health.
Monitoring Hormone Levels:
- Regular blood tests to monitor hormone levels (including estrogen and testosterone) can provide valuable information about the hormonal balance during a cycle.
- Adjustments to medication dosages can be made based on the results.
Avoiding Excessive Dosages and Duration:
- Using moderate dosages of anabolic steroids and limiting the duration of cycles can help minimise the risk of side effects, including gynecomastia.
Choosing Steroids with Lower Aromatisation:
- Some anabolic steroids have a lower tendency to convert to estrogen. Choosing steroids with lower aromatisation potential can help reduce the risk of estrogen-related side effects.
Post-Cycle Therapy (PCT):
- Incorporating a proper post-cycle therapy protocol after completing a cycle can help restore hormonal balance and reduce the risk of gynecomastia and other side effects.
Does gyno hurt?
Gynecomastia, typically doesn’t cause physical pain or discomfort for most individuals. In many cases, gynecomastia is painless and is more of a cosmetic concern. The breast tissue that develops is typically soft and glandular in nature, similar to the breast tissue in females.
However, there are some situations where gynecomastia might be associated with discomfort or pain:
Sensitive or Tender Breasts: Some individuals with gynecomastia may experience sensitivity or tenderness in the breast area. This sensitivity can be more pronounced during certain periods, such as during puberty or when hormonal changes occur.
Underlying Medical Conditions: Gynecomastia caused by certain medical conditions, such as a hormonal imbalance or a tumor affecting the endocrine system, could be associated with discomfort or pain. However, gynecomastia itself is not typically the primary cause of pain in these cases.
Inflammatory or Infection-Related Issues: In rare cases, inflammation or infection of the breast tissue can occur, leading to pain or discomfort. This is not a common feature of typical gynecomastia.
Psychological Distress: While not physical pain, gynecomastia can lead to emotional discomfort, self-consciousness, and psychological distress due to body image concerns. This emotional impact can cause significant distress even in the absence of physical pain.
If you are experiencing discomfort, pain, or tenderness in the breast area, it’s important to consult a healthcare professional for an accurate diagnosis and appropriate guidance.